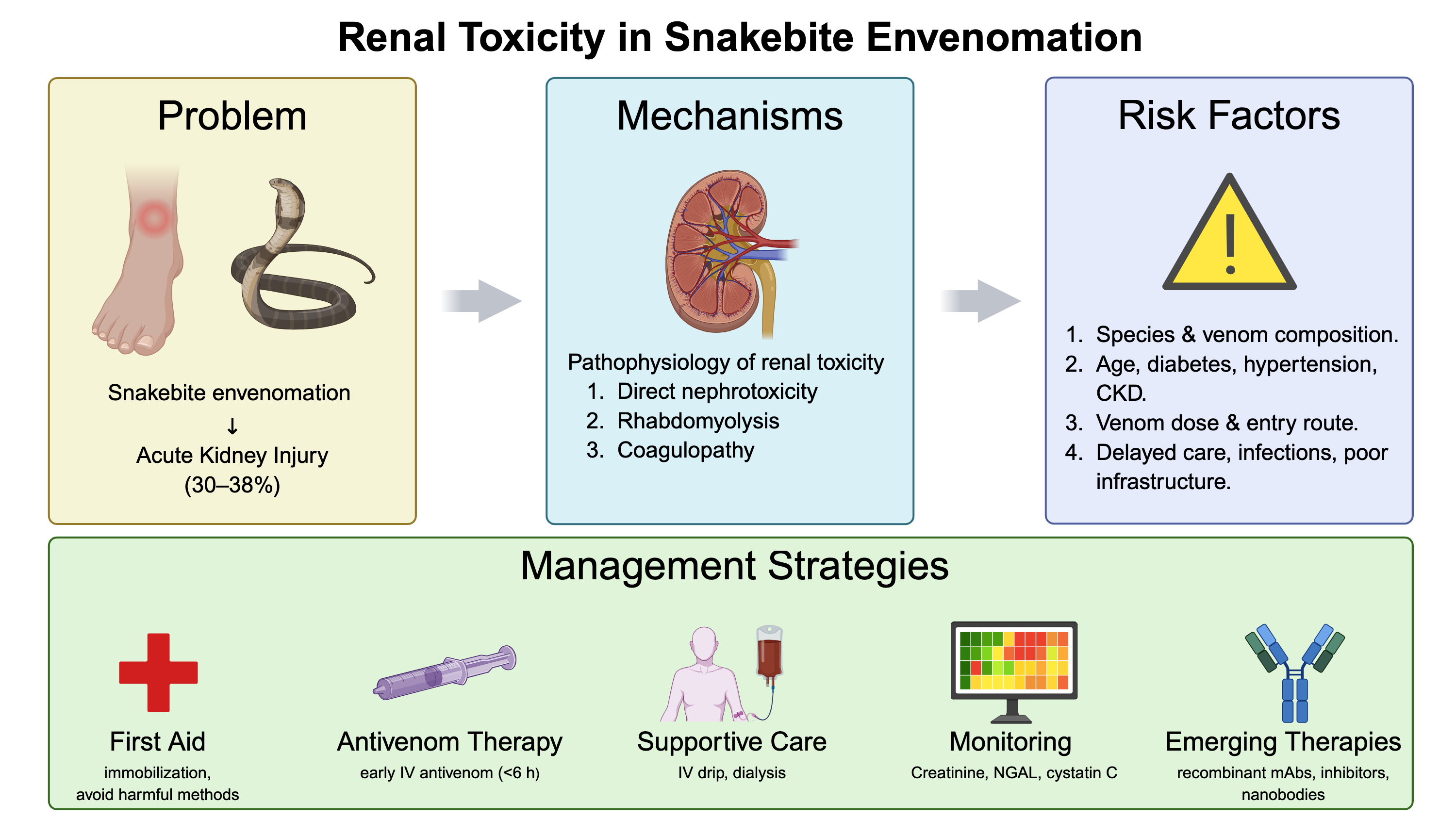
Renal Toxicity in Snakebite Envenomation: Insights into Pathophysiology, Risk Factors, and Management Strategies
DOI:
https://doi.org/10.59796/jcst.V15N4.2025.138Keywords:
acute kidney injury, antivenom therapy, renal toxicity, snakebite envenomation, venom nephrotoxicityAbstract
Renal toxicity is one of the most severe complications associated with snakebite envenomation, contributing significantly to morbidity and mortality among affected individuals. This review provides a comprehensive analysis of renal toxicity in snakebite victims, focusing on the underlying pathophysiological mechanisms, risk factors, and current management strategies. Snake venom-induced renal damage may occur through various mechanisms, including direct nephrotoxicity, rhabdomyolysis, and coagulopathy. The extent of renal injury is influenced by factors such as venom composition, dosage, route of entry, and the victim’s pre-existing health conditions. We also conducted a bibliometric analysis of research trends in this field, highlighting a growing body of literature that reflects increased awareness of snakebite-associated renal complications and advancements in research methodologies. This review synthesizes current knowledge on the prevention and treatment of venom-induced renal toxicity, emphasizing the importance of early intervention, supportive care, and appropriate antivenom therapy. Furthermore, it identifies gaps in existing research and proposes future directions to enhance the understanding and management of renal complications caused by snake envenomation. These insights aim to improve patient outcomes and inform clinical practices in regions with a high prevalence of snakebite envenomation.
References
Adams, A. C., Grav, L. M., Ahmadi, S., Holst Dahl, C., Ljungars, A., Laustsen, A. H., & Nielsen, L. K. (2024). Single‐batch expression of an experimental recombinant snakebite antivenom based on an oligoclonal mixture of human monoclonal antibodies. Biotechnology Journal, 19(10), Article e202400348. https://doi.org/10.1002/biot.202400348
Afroz, A., Siddiquea, B. N., Chowdhury, H. A., Jackson, T. N., & Watt, A. D. (2024). Snakebite envenoming: A systematic review and meta-analysis of global morbidity and mortality. PLoS Neglected Tropical Diseases, 18(4), Article e0012080. https://doi.org/10.1371/journal.pntd.0012080
Afroz, A., Siddiquea, B. N., Shetty, A. N., Jackson, T. N., & Watt, A. D. (2023). Assessing knowledge and awareness regarding snakebite and management of snakebite envenoming in healthcare workers and the general population: A systematic review and meta-analysis. PLOS Neglected Tropical Diseases, 17(2), Article e0011048. https://doi.org/10.1371/journal.pntd.0011048
Alangode, A., Rajan, K., & Nair, B. G. (2020). Snake antivenom: Challenges and alternate approaches. Biochemical Pharmacology, 181, Article 114135. https://doi.org/10.1016/j.bcp.2020.114135
Albulescu, L. O., Xie, C., Ainsworth, S., Alsolaiss, J., Crittenden, E., Dawson, C. A., ... & Casewell, N. R. (2020). A therapeutic combination of two small molecule toxin inhibitors provides broad preclinical efficacy against viper snakebite. Nature Communications, 11(1), Article 6094. https://doi.org/10.1038/s41467-020-19981-6
Albuquerque, P. L. M. M., Da Silva Jr, G., Meneses, G. C., Martins, A. M. C., Raubenheimer, J., Shihana, F., ... & Daher, E. F. (2019a). SAT-158 renal tubular dysfunction, coagulation disturbances and novel biomarkers in acute kidney injury due to snakebites. Kidney International Reports, 4(7), Article S71. https://doi.org/10.1016/j.ekir.2019.05.190
Albuquerque, P. L. M. M., da Silva Junior, G. B., Meneses, G. C., Martins, A. M. C., Lima, D. B., Raubenheimer, J., ... & Daher, E. D. F. (2019b). Acute kidney injury induced by Bothrops venom: Insights into the pathogenic mechanisms. Toxins, 11(3), Article 148. https://doi.org/10.3390/toxins11030148
Alirahimi, E., Kazemi-Lomedasht, F., Shahbazzadeh, D., Habibi-Anbouhi, M., Chafi, M. H., Sotoudeh, N., ... & Behdani, M. (2018). Nanobodies as novel therapeutic agents in envenomation. Biochimica et Biophysica Acta (BBA)-General Subjects, 1862(12), 2955-2965. https://doi.org/10.1016/j.bbagen.2018.08.019
Alirol, E., Sharma, S. K., Ghimire, A., Poncet, A., Combescure, C., Thapa, C., ... & Chappuis, F. (2017). Dose of antivenom for the treatment of snakebite with neurotoxic envenoming: Evidence from a randomised controlled trial in Nepal. PLoS Neglected Tropical Diseases, 11(5), Article e0005612. https://doi.org/10.1371/journal.pntd.0005612
Alvitigala, B. Y., Gooneratne, L. V., Gnanathasan, C. A., & Wijewickrama, E. S. (2025). Snakebite-associated acute kidney injury in South Asia: Narrative review on epidemiology, pathogenesis and management. Transactions of The Royal Society of Tropical Medicine and Hygiene, 119(6), 648-664. https://doi.org/10.1093/trstmh/trae077
Aphrodita, A., Sentono, D. N., Yudha, D. S., Purwestri, Y. A., Nuringtyas, T. R., Raharjo, S., ... & Sofyantoro, F. (2025). Comparative analysis of hemotoxic, myotoxic, and inflammatory profiles of Calloselasma rhodostoma and Trimeresurus insularis venoms in mice. Narra J, 5(2), e1874-e1874. https://doi.org/10.52225/narraj.v5i2.1874
Arbel, Y., Ben-Assa, E., Puzhevsky, D., Litmanowicz, B., Galli, N., Chorin, E., ... & Finkelstein, A. (2019). Forced diuresis with matched hydration during transcatheter aortic valve implantation for reducing acute kidney injury: A randomized, sham-controlled study (REDUCE-AKI). European Heart Journal, 40(38), 3169-3178. https://doi.org/10.1093/eurheartj/ehz343
Avau, B., Borra, V., Vandekerckhove, P., & De Buck, E. (2016). The treatment of snake bites in a first aid setting: A systematic review. PLoS Neglected Tropical Diseases, 10(10), Article e0005079. https://doi.org/10.1371/journal.pntd.0005079
Azevedo-Marques, M. M., Cupo, P., Coimbra, T. M., Hering, S. E., Rossi, M. A., & Laure, C. J. (1985). Myonecrosis, myoglobinuria and acute renal failure induced by South American rattlesnake (Crotalus durissus terrificus) envenomation in Brazil. Toxicon, 23(4), 631-636. https://doi.org/10.1016/0041-0101(85)90367-8
Barnes, K., Ngari, C., Parkurito, S., Wood, L., Otundo, D., Harrison, R., ... & Baker, C. (2021). Delays, fears and training needs: Perspectives of health workers on clinical management of snakebite revealed by a qualitative study in Kitui County, Kenya. Toxicon: X, 11, Article 100078. https://doi.org/10.1016/j.toxcx.2021.100078
Bhuvaneshwari, B., & Umarani, U. (2022). A study of incidence of acute kidney injury in snake bite. Global Journal for Research Analysis, 11(12), 34–37. https://doi.org/10.36106/gjra/1307569
Bickler, P. E. (2020). Amplification of snake venom toxicity by endogenous signaling pathways. Toxins, 12(2), Article 68. https://doi.org/10.3390/toxins12020068
Boer-Lima, P. A., & Cruz-HÃ, M. A. (2002). Bothrops moojeni snake venom-induced renal glomeruli changes in rat. The American Journal of Tropical Medicine and Hygiene, 67(2), 217-222. https://doi.org/10.4269/ajtmh.2002.67.217
Bonilla-Aldana, D. K., Bonilla-Aldana, J. L., Ulloque-Badaracco, J. R., Al-kassab-Córdova, A., Hernandez-Bustamante, E. A., Alarcon-Braga, E. A., ... & Suarez, J. A. (2024). Snakebite-associated infections: A systematic review and meta-analysis. The American Journal of Tropical Medicine and Hygiene, 110(5), Article 874. https://doi.org/10.4269/ajtmh.23-0278
Braga, J. R. M., Jorge, A. R. C., Marinho, A. D., de Moraes Silveira, J. A., Nogueira-Junior, F. A., Valle, M. B., ... & Jorge, R. J. B. (2020). Renal effects of venoms of Mexican coral snakes Micrurus browni and Micrurus laticollaris. Toxicon, 181, 45-52. https://doi.org/10.1016/j.toxicon.2020.04.095
Bush, S. P. (2004). Snakebite suction devices don't remove venom: They just suck. Annals of Emergency Medicine, 43(2), 187-188. https://doi.org/10.1016/j.annemergmed.2003.10.031
Bustillo, S., García-Denegri, M. E., Gay, C., Van de Velde, A. C., Acosta, O., Angulo, Y., ... & Leiva, L. (2015). Phospholipase A2 enhances the endothelial cell detachment effect of a snake venom metalloproteinase in the absence of catalysis. Chemico-biological Interactions, 240, 30-36. https://doi.org/10.1016/j.cbi.2015.08.002
Cai, Q., Jing, R., Zhang, W., Tang, Y., Li, X., & Liu, T. (2020). Hydration strategies for preventing contrast‐induced acute kidney injury: A systematic review and bayesian network meta‐analysis. Journal of Interventional Cardiology, 2020(1), Article 7292675. https://doi.org/10.1155/2020/7292675
Cavalcante, T. T. A., de Souza, M. B. S., Neves, J. C. F., Ibiapina, H. N. S., Barbosa, F. B. A., Bentes, K. O., ... & Sartim, M. A. (2023). Inflammatory profile associated with secondary infection from bothrops atrox snakebites in the Brazilian amazon. Toxins, 15(9), Article 524. https://doi.org/10.3390/toxins15090524
Chaaithanya, I. K., Abnave, D., Bawaskar, H., Pachalkar, U., Tarukar, S., Salvi, N., ... & Gajbhiye, R. K. (2021). Perceptions, awareness on snakebite envenoming among the tribal community and health care providers of Dahanu block, Palghar District in Maharashtra, India. Plos One, 16(8), Article e0255657. https://doi.org/10.1371/journal.pone.0255657
Chaisakul, J., Alsolaiss, J., Charoenpitakchai, M., Wiwatwarayos, K., Sookprasert, N., Harrison, R. A., ... & Casewell, N. R. (2019). Evaluation of the geographical utility of Eastern Russell’s viper (Daboia siamensis) antivenom from Thailand and an assessment of its protective effects against venom-induced nephrotoxicity. PLoS Neglected Tropical Diseases, 13(10), Article e0007338. https://doi.org/10.1371/journal.pntd.0007338
Chaisakul, J., Khow, O., Wiwatwarayos, K., Rusmili, M. R. A., Prasert, W., Othman, I., ... & Chaiyabutr, N. (2021). A biochemical and pharmacological characterization of phospholipase A2 and metalloproteinase fractions from Eastern Russell’s viper (Daboia siamensis) venom: Two major components associated with acute kidney injury. Toxins, 13(8), Article 521. https://doi.org/10.3390/toxins13080521
Chaisakul, J., Rusmili, M. R. A., Alsolaiss, J., Albulescu, L. O., Harrison, R. A., Othman, I., & Casewell, N. R. (2020). In vitro immunological cross-reactivity of Thai polyvalent and monovalent antivenoms with Asian viper venoms. Toxins, 12(12), Article 766. https://doi.org/10.3390/toxins12120766
Chaiyabutr, N., Chanhome, L., Vasaruchapong, T., Laoungbua, P., Khow, O., Rungsipipat, A., ... & Sitprija, V. (2022). Comparative compositional and functional venomic profiles among venom specimens from juvenile, subadult and adult Russell’s viper (Daboia siamensis): Correlation with renal pathophysiology in experimental rabbits. Journal of Venomous Animals and Toxins including Tropical Diseases, 28, Article 20210111. https://doi.org/10.1590/1678-9199-JVATITD-2021-0111
Chaves, F., Gutiérrez, J., & Brenes, F. (1992). Pathological and biochemical changes induced in mice after intramuscular injection of venom from newborn specimens of the snake Bothrops asper (Terciopelo). Toxicon, 30(9), 1099-1109. https://doi.org/10.1016/0041-0101(92)90055-A
Chuang, P. C., Chang, K. W., Cheng, S. Y., Pan, H. Y., Huang, K. C., Huang, Y. T., & Li, C. J. (2021). Benefits of early in-hospital antivenom administration to patients with Protobothrops mucrosquamatus envenomation. The American Journal of Tropical Medicine and Hygiene, 104(1), Article 323. https://doi.org/10.4269/ajtmh.20-0659
Chugh, K. S. (1989). Snake-bite-induced acute renal failure in India. Kidney International, 35(3), 891-907. https://doi.org/10.1038/ki.1989.70
da Silva, T. B., Aly, J., Figueira, M., da Gama Araújo, C. M., de Sousa, I. K. F., Tonin, A. A., ... & dos Santos Sousa, R. (2021). Epidemiological aspects of snakebites in the state of Amazonas, Brazil, from 2007 to 2017. Revista de Patologia Tropical/Journal of Tropical Pathology, 50(4), 315-326. https://doi.org/10.5216/rpt.v50i4.67841
Dineshkumar, T., Dhanapriya, J., Murugananth, S., Surendar, D., Sakthirajan, R., Rajasekar, D., ... & Gopalakrishnan, N. (2018). Snake envenomation-induced acute interstitial nephritis. Integrative Medicine in Nephrology and Andrology, 5(1), 14-17.
Engel, C. E. (1979). How can you decide what to teach?. Medical Journal of Australia, 1(10), 438-440. https://doi.org/10.5694/j.1326-5377.1979.tb127021.x
Gajbhiye, R. K., Chaaithanya, I. K., Munshi, H., Prusty, R. K., Mahapatra, A., Palo, S. K., ... & Mahale, S. D. (2023). National snakebite project on capacity building of health system on prevention and management of snakebite envenoming including its complications in selected districts of Maharashtra and Odisha in India: A study protocol. PLoS One, 18(2), Article e0281809. https://doi.org/10.1371/journal.pone.0281809
Gamulin, E., Mateljak Lukačević, S., Halassy, B., & Kurtović, T. (2023). Snake antivenoms-toward better understanding of the administration route. Toxins, 15(6), Article 398. https://doi.org/10.3390/toxins15060398
Gois, P. H. F., Martines, M. S., Ferreira, D., Volpini, R., Canale, D., Malaque, C., ... & Seguro, A. C. (2017). Allopurinol attenuates acute kidney injury following Bothrops jararaca envenomation. PLoS Neglected Tropical Diseases, 11(11), Article e0006024. https://doi.org/10.1371/journal.pntd.0006024
Gutiérrez, J. M., Burnouf, T., Harrison, R. A., Calvete, J. J., Kuch, U., Warrell, D. A., & Williams, D. J. (2014). A multicomponent strategy to improve the availability of antivenom for treating snakebite envenoming. Bulletin of the World Health Organization, 92(7), 526-532. https://doi.org/10.2471/BLT.13.132431
Gutiérrez, J. M., Calvete, J. J., Habib, A. G., Harrison, R. A., Williams, D. J., & Warrell, D. A. (2017a). Snakebite envenoming. Nature Reviews Disease Primers, 3(1), 1-21. https://doi.org/10.1038/nrdp.2017.63
Gutiérrez, J. M., Escalante, T., & Rucavado, A. (2009). Experimental pathophysiology of systemic alterations induced by Bothrops asper snake venom. Toxicon, 54(7), 976-987. https://doi.org/10.1016/j.toxicon.2009.01.039
Gutiérrez, J. M., Solano, G., Pla, D., Herrera, M., Segura, Á., Vargas, M., ... & Calvete, J. J. (2017b). Preclinical evaluation of the efficacy of antivenoms for snakebite envenoming: State-of-the-art and challenges ahead. Toxins, 9(5), Article 163. https://doi.org/10.3390/toxins9050163
Hamza, M., Knudsen, C., Gnanathasan, C. A., Monteiro, W., Lewin, M. R., Laustsen, A. H., & Habib, A. G. (2021). Clinical management of snakebite envenoming: Future perspectives. Toxicon: X, 11, Article 100079. https://doi.org/10.1016/j.toxcx.2021.100079
Herath, H. M. N. J., Wazil, A. W. M., Abeysekara, D. T. D. J., Jeewani, N. D. C., Weerakoon, K. G. A. D., Ratnatunga, N. V. I., ... & Kularatne, S. A. M. (2012). Chronic kidney disease in snake envenomed patients with acute kidney injury in Sri Lanka: A descriptive study. Postgraduate Medical Journal, 88(1037), 138-142. https://doi.org/10.1136/postgradmedj-2011-130225
Horo, S. M., Mardi, V., Shankar Munda, S., & Minz, G. (2022). Study of clinical profile of acute renal failure in snake bite patients. Global Journal for Research Analysis, 11(2), 26–27. https://doi.org/10.36106/gjra/6200978
Houcke, S., Pujo, J. M., Vauquelin, S., Lontsi Ngoula, G. R., Matheus, S., Nkontcho, F., ... & Kallel, H. (2023). Effect of the time to antivenom administration on recovery from snakebite envenoming-related coagulopathy in French Guiana. PLoS Neglected Tropical Diseases, 17(4), Article e0011242. https://doi.org/10.1371/journal.pntd.0011242
Iliyasu, G., Tiamiyu, A. B., Daiyab, F. M., Tambuwal, S. H., Habib, Z. G., & Habib, A. G. (2015). Effect of distance and delay in access to care on outcome of snakebite in rural north-eastern Nigeria. Rural and Remote Health, 15(4), 76-81. https://doi.org/10.22605/RRH3496
Isbister, G. K. (2010). Snakebite doesn't cause disseminated intravascular coagulation: coagulopathy and thrombotic microangiopathy in snake envenoming. In Seminars in Thrombosis and Hemostasis, 36(4), 444-451. https://doi.org/10.1055/s-0030-1254053
Isbister, G. K. (2023). Antivenom availability, delays and use in Australia. Toxicon: X, 17, Article 100145. https://doi.org/10.1016/j.toxcx.2022.100145
Isbister, G. K. (2024). The critical time period for administering antivenom: Golden hours and missed opportunities. Clinical Toxicology, 62(5), 277-279. https://doi.org/10.1080/15563650.2024.2352026
Isbister, G. K., Brown, S. G., Page, C. B., McCoubrie, D. L., Greene, S. L., & Buckley, N. A. (2013). Snakebite in Australia: A practical approach to diagnosis and treatment. Medical Journal of Australia, 199(11), 763-768. https://doi.org/10.5694/mja12.11172
Islam, K., Seth, S., Roy, A., & Datta, A. K. (2020). Predictors of renal complications in children with hematotoxic snakebite. Indian Pediatrics, 57(5), 427-430. https://doi.org/10.1007/s13312-020-1817-7
Kanjanabuch, T., & Sitprija, V. (2008, July). Snakebite nephrotoxicity in Asia. In Seminars in Nephrology, 28(4), 363-372. https://doi.org/10.1016/j.semnephrol.2008.04.005
Kasturiratne, A., Wickremasinghe, A. R., De Silva, N., Gunawardena, N. K., Pathmeswaran, A., Premaratna, R., ... & De Silva, H. J. (2008). The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Medicine, 5(11), Article e218. https://doi.org/10.1371/journal.pmed.0050218
Khalek, I. S., Senji Laxme, R. R., Nguyen, Y. T. K., Khochare, S., Patel, R. N., Woehl, J., ... & Jardine, J. G. (2024). Synthetic development of a broadly neutralizing antibody against snake venom long-chain α-neurotoxins. Science Translational Medicine, 16(735), Article eadk1867. https://doi.org/10.1126/scitranslmed.adk1867
Khimmaktong, W., Nuanyaem, N., Lorthong, N., Hodgson, W. C., & Chaisakul, J. (2022). Histopathological changes in the liver, heart and kidneys following Malayan pit viper (Calloselasma rhodostoma) envenoming and the neutralising effects of hemato polyvalent snake antivenom. Toxins, 14(9), Article 601. https://doi.org/10.3390/toxins14090601
Knudsen, C., & Laustsen, A. H. (2018). Recent advances in next generation snakebite antivenoms. Tropical Medicine and Infectious Disease, 3(2), Article 42. https://doi.org/10.3390/tropicalmed3020042
Kumar, M., Arcot Thanjan, M., Gopalakrishnan, N., Jeyachandran, D., Thanigachalam, D., & Ramanathan, S. (2022). Snake envenomation-induced acute kidney injury: Prognosis and long-term renal outcomes. Postgraduate Medical Journal, 98(1158), 264-268. https://doi.org/10.1136/postgradmedj-2020-139021
Kusuma, W. A., Fadli, A., Fatriani, R., Sofyantoro, F., Yudha, D. S., Lischer, K., ... & Swasono, R. T. (2023). Prediction of the interaction between Calloselasma rhodostoma venom-derived peptides and cancer-associated hub proteins: A computational study. Heliyon, 9(11), Article e21149. https://doi.org/10.1016/j.heliyon.2023.e21149
Laustsen, A. H., Gless, B. H., Jenkins, T. P., Meyhoff-Madsen, M., Bjärtun, J., Munk, A. S., ... & Lohse, B. (2022). In vivo neutralization of myotoxin II, a phospholipase A2 homologue from Bothrops asper venom, using peptides discovered via phage display technology. ACS Omega, 7(18), 15561-15569. https://doi.org/10.1021/acsomega.2c00280
Ledsgaard, L., Laustsen, A. H., Pus, U., Wade, J., Villar, P., Boddum, K., ... & Karatt-Vellatt, A. (2022). In vitro discovery of a human monoclonal antibody that neutralizes lethality of cobra snake venom. Mabs, 14(1), Article 2085536. https://doi.org/10.1080/19420862.2022.2085536
Ledsgaard, L., Wade, J., Jenkins, T. P., Boddum, K., Oganesyan, I., Harrison, J. A., ... & Karatt-Vellatt, A. (2023). Discovery and optimization of a broadly-neutralizing human monoclonal antibody against long-chain α-neurotoxins from snakes. Nature Communications, 14(1), Article 682. https://doi.org/10.1038/s41467-023-36393-4
Lentz, T. L., Hawrot, E., & Wilson, P. T. (1987). Synthetic peptides corresponding to sequences of snake venom neurotoxins and rabies virus glycoprotein bind to the nicotinic acetylcholine receptor. Proteins: Structure, Function, and Bioinformatics, 2(4), 298-307. https://doi.org/10.1002/prot.340020406
Levey, A. S., & James, M. T. (2017). Acute Kidney Injury. Annals of Internal Medicine, 167(9), Article ITC66. https://doi.org/10.7326/AITC201711070
Li, X., Liu, C., Mao, Z., Li, Q., & Zhou, F. (2021). Timing of renal replacement therapy initiation for acute kidney injury in critically ill patients: a systematic review of randomized clinical trials with meta-analysis and trial sequential analysis. Critical Care, 25(1), Article 15. https://doi.org/10.1186/s13054-020-03451-y
Maciel Salazar, G. K., Saturnino Cristino, J., Vilhena Silva-Neto, A., Seabra Farias, A., Alcântara, J. A., Azevedo Machado, V., ... & Sachett, J. (2021). Snakebites in “Invisible Populations”: A cross-sectional survey in riverine populations in the remote western Brazilian Amazon. PLoS Neglected Tropical Diseases, 15(9), Article e0009758. https://doi.org/10.1371/journal.pntd.0009758
Mahmood, M. A., Halliday, D., Cumming, R., Thwin, K. T., Myitzu, M., White, J., ... & Peh, C. A. (2019). Inadequate knowledge about snakebite envenoming symptoms and application of harmful first aid methods in the community in high snakebite incidence areas of Myanmar. PLoS Neglected Tropical Diseases, 13(2), Article e0007171. https://doi.org/10.1371/journal.pntd.0007171
Marinho, A. D., de Moraes Silveira, J. A., Chaves Filho, A. J. M., Jorge, A. R. C., Júnior, F. A. N., Pereira, V. B. M., ... & Monteiro, H. S. A. (2021). Bothrops pauloensis snake venom-derived Asp-49 and Lys-49 phospholipases A2 mediates acute kidney injury by oxidative stress and release of inflammatory cytokines. Toxicon, 190, 31-38. https://doi.org/10.1016/j.toxicon.2020.12.004
Masci, P. P., Rowe, E. A., Whitaker, A. N., & De Jersey, J. (1990). Fibrinolysis as a feature of disseminated intravascular coagulation (DIC) after Pseudonaja textilis textilis envenomation. Thrombosis Research, 59(5), 859-870. https://doi.org/10.1016/0049-3848(90)90399-W
Mejri, H., Mokrani, R., Ksouri, A., Seddik, M., Awad, N., Ayme, G., ... & Bouhaouala-Zahar, B. (2024). Neutralizing nanobodies against venoms from Naja haje species captured in north africa. Toxins, 16(9), Article 393. https://doi.org/10.3390/toxins16090393
Menzies, S. K., Patel, R. N., & Ainsworth, S. (2025). Practical progress towards the development of recombinant antivenoms for snakebite envenoming. Expert Opinion on Drug Discovery, 20(6), 799-819. https://doi.org/10.1080/17460441.2025.2495943
Michael, G. C., Thacher, T. D., & Shehu, M. I. (2011). The effect of pre-hospital care for venomous snake bite on outcome in Nigeria. Transactions of the Royal Society of Tropical Medicine and Hygiene, 105(2), 95-101. https://doi.org/10.1016/j.trstmh.2010.09.005
Monteiro, W. M., Farias, A. S. D., Val, F., Neto, A. V. S., Sachett, A., Lacerda, M., ... & Wen, F. H. (2020). Providing antivenom treatment access to all Brazilian Amazon indigenous areas: ‘Every life has equal value’. Toxins, 12(12), Article 772. https://doi.org/10.3390/toxins12120772
Nduwayezu, R., Kinney, H., Amuguni, J. H., & Schurer, J. M. (2020). Snakebite envenomation in Rwanda: Patient demographics, medical care, and antivenom availability in the formal healthcare sector. The American Journal of Tropical Medicine and Hygiene, 104(1), Article 316. https://doi.org/10.4269/ajtmh.20-0976
Nirja, K., & Rathore, S. S. (2020). Risk factor analysis for acute kidney injury in snake bite: Retrospective study from Western Rajasthan. Scholars Journal of Applied Medical Sciences, 08(04), 1098–1101.
Noutsos, T., Currie, B. J., Isoardi, K. Z., Brown, S. G., & Isbister, G. K. (2022a). Snakebite-associated thrombotic microangiopathy: An Australian prospective cohort study [ASP30]. Clinical Toxicology, 60(2), 205-213. https://doi.org/10.1080/15563650.2021.1948559
Noutsos, T., Currie, B. J., Lek, R. A., & Isbister, G. K. (2020). Snakebite associated thrombotic microangiopathy: A systematic review of clinical features, outcomes, and evidence for interventions including plasmapheresis. PLoS Neglected Tropical Diseases, 14(12), Article e0008936. https://doi.org/10.1371/journal.pntd.0008936
Noutsos, T., Currie, B. J., Wijewickrama, E. S., & Isbister, G. K. (2022b). Snakebite associated thrombotic microangiopathy and recommendations for clinical practice. Toxins, 14(1), Article 57. https://doi.org/10.3390/toxins14010057
Oukkache, N., Jaoudi, R. E., Ghalim, N., Chgoury, F., Bouhaouala, B., Mdaghri, N. E., & Sabatier, J. M. (2014). Evaluation of the lethal potency of scorpion and snake venoms and comparison between intraperitoneal and intravenous injection routes. Toxins, 6(6), 1873-1881. https://doi.org/10.3390/toxins6061873
Parihar, V., Mittal, A., Vikarn, V., Didel, S., & Singh, K. (2023). Venom-induced consumptive coagulopathy leading to thrombotic microangiopathy following Echis carinatus sochureki bite: Is snake antivenom effective?. Journal of Tropical Pediatrics, 69(1), Article fmac113. https://doi.org/10.1093/tropej/fmac113
Parker-Cote, J., & Meggs, W. J. (2018). First aid and pre-hospital management of venomous snakebites. Tropical Medicine and Infectious Disease, 3(2), Article 45. https://doi.org/10.3390/tropicalmed3020045
Patil, S., Paranjape, A., Patil, N. R., Patil, H. S., Surve, R. A., & Desai, M. B. (2019). Rural set up experience of viper bite treatment with special reference to FFP in venom induced consumption coagulopathy. The Journal of the Association of Physicians of India, 67(10), 26-28.
Patra, A., & Mukherjee, A. K. (2021). Assessment of snakebite burdens, clinical features of envenomation, and strategies to improve snakebite management in Vietnam. Acta Tropica, 216, Article 105833. https://doi.org/10.1016/j.actatropica.2021.105833
Pechprasarn, S., Wetchasit, P., & Pongsuwan, S. (2025). Optimizing chronic kidney disease prediction: A machine learning approach with minimal diagnostic predictors. Journal of Current Science and Technology, 15(1), Article 76. https://doi.org/10.59796/jcst.V15N1.2025.76
Plackett, R., Kaushal, A., Kassianos, A. P., Cross, A., Lewins, D., Sheringham, J., ... & von Wagner, C. (2020). Use of social media to promote cancer screening and early diagnosis: Scoping review. Journal of Medical Internet Research, 22(11), Article e21582. https://doi.org/10.2196/21582
Ponraj, D., & Gopalakrishnakone, P. (1995). Morphological changes induced by a generalized myotoxin (myoglobinuria-inducing toxin) from the venom of Pseudechis australis (king brown snake) in skeletal muscle and kidney of mice. Toxicon, 33(11), 1453-1467. https://doi.org/10.1016/0041-0101(95)00091-Y
Priyamvada, P. S., Jaswanth, C., Zachariah, B., Haridasan, S., Parameswaran, S., & Swaminathan, R. P. (2020). Prognosis and long-term outcomes of acute kidney injury due to snake envenomation. Clinical Kidney Journal, 13(4), 564-570. https://doi.org/10.1093/ckj/sfz055
Prowle, J. R., Chua, H. R., Bagshaw, S. M., & Bellomo, R. (2012). Clinical review: Volume of fluid resuscitation and the incidence of acute kidney injury-a systematic review. Critical Care, 16(4), Article 230. https://doi.org/10.1186/cc11345
Prowle, J. R., Kirwan, C. J., & Bellomo, R. (2014). Fluid management for the prevention and attenuation of acute kidney injury. Nature Reviews Nephrology, 10(1), 37-47. https://doi.org/10.1038/nrneph.2013.232
Pujo, J. M., Houcke, S., Ngoulla, G. R. L., Laurent, V., Signaté, B., Mutricy, R., ... & Kallel, H. (2025). Effectiveness of late and very late antivenom administration on recovery from snakebite-induced coagulopathy in French Guiana: A population-based study. The Lancet Regional Health–Americas, 42. Article 100994. https://doi.org/10.1016/j.lana.2025.100994
Rao, P. S. K., Priyamvada, P. S., & Bammigatti, C. (2025). Snakebite envenomation-associated acute kidney injury: A South-Asian perspective. Transactions of The Royal Society of Tropical Medicine and Hygiene, 119(7), Article trae114. https://doi.org/10.1093/trstmh/trae114
Ratanabanangkoon, K. (2023). Polyvalent snake antivenoms: Production strategy and their therapeutic benefits. Toxins, 15(9), Article 517. https://doi.org/10.3390/toxins15090517
Rathnayaka, R. M. M. K., Ranathunga, P. E. A. N., & Kularatne, S. A. M. (2021). Thrombotic microangiopathy, hemolytic uremic syndrome and thrombotic thrombocytopenic purpura: Rare manifestations of Russell’s viper (Daboia russelii) envenoming in Sri Lanka. Asia Pacific Journal of Medical Toxicology, 10(3), 117-123. https://doi.org/10.22038/apjmt.2021.18818
Ratnayake, I., Mohamed, F., Buckley, N. A., Gawarammana, I. B., Dissanayake, D. M., Chathuranga, U., ... & Isbister, G. K. (2019). Early identification of acute kidney injury in Russell’s viper (Daboia russelii) envenoming using renal biomarkers. PLoS Neglected Tropical Diseases, 13(7), Article e0007486. https://doi.org/10.1371/journal.pntd.0007486
Resiere, D., Mehdaoui, H., & Gutiérrez, J. M. (2018). Snakebite envenomation in the Caribbean: The role of medical and scientific cooperation. PLoS Neglected Tropical Diseases, 12(7), Article e0006441. https://doi.org/10.1371/journal.pntd.0006441
Ryan, S. E., & Yong, J. L. (2002). Acute myotoxic and nephrotoxic effects of Aipysurus laevis venom following intramuscular injection in mice. Experimental and Toxicologic Pathology, 54(1), 61-67. https://doi.org/10.1078/0940-2993-00232
Saladini, L. Y., Magalhães-Junior, M. J., da Silva, C. C. F., Oliveira, P. G. C., Kodama, R. T., Gomes, L., ... & Portaro, F. C. V. (2024). Evaluation of the inhibitory potential of synthetic peptides homologous to CDR3 regions of a monoclonal antibody against Bothropic venom serine proteases. International Journal of Molecular Sciences, 25(10), Article 5181. https://doi.org/10.3390/ijms25105181
Salah Eldin, H., & Hafez, R. (2017). Clinical and laboratory parameters associated with acute kidney injury in viper envenomed cases. Ain Shams Journal of Forensic Medicine and Clinical Toxicology, 29(2), 80-88. https://doi.org/10.21608/ajfm.2017.18212
Samuel, S. P., Chinnaraju, S., Williams, H. F., Pichamuthu, E., Subharao, M., Vaiyapuri, M., ... & Vaiyapuri, S. (2020). Venomous snakebites: Rapid action saves lives a multifaceted community education programme increases awareness about snakes and snakebites among the rural population of Tamil Nadu, India. PLoS Neglected Tropical Diseases, 14(12), Article e0008911. https://doi.org/10.1371/journal.pntd.0008911
Sanhajariya, S., Duffull, S. B., & Isbister, G. K. (2018). Pharmacokinetics of snake venom. Toxins, 10(2), Article 73. https://doi.org/10.3390/toxins10020073
Sarkar, S., Sinha, R., Chaudhury, A. R., Maduwage, K., Abeyagunawardena, A., Bose, N., ... & McCulloch, M. (2021). Snake bite associated with acute kidney injury. Pediatric Nephrology, 36(12), 3829-3840. https://doi.org/10.1007/s00467-020-04911-x
Sartim, M. A., Cezarette, G. N., Jacob-Ferreira, A. L., Frantz, F. G., Faccioli, L. H., & Sampaio, S. V. (2017). Disseminated intravascular coagulation caused by moojenactivase, a procoagulant snake venom metalloprotease. International Journal of Biological Macromolecules, 103, 1077-1086. https://doi.org/10.1016/j.ijbiomac.2017.05.146
Senthilkumaran, S., Patel, K., Salim, A., Vijayakumar, P., Williams, H. F., Vaiyapuri, R., ... & Vaiyapuri, S. (2021). Neutrophil gelatinase–associated lipocalin acts as a robust early diagnostic marker for renal replacement therapy in patients with Russell’s viper bite–induced acute kidney injuries. Toxins, 13(11), Article 797. https://doi.org/10.3390/toxins13110797
Shankar, T., Arora, P., Jose, J. R., & Kaushik, A. (2024). Thrombotic microangiopathy following a white-lipped pit viper envenomation. BMJ Case Reports CP, 17(5), Article e258813. https://doi.org/10.1136/bcr-2023-258813
Sharma, N., Chauhan, S., Faruqi, S., Bhat, P., & Varma, S. (2005). Snake envenomation in a north Indian hospital. Emergency Medicine Journal, 22(2), 118-120. https://doi.org/10.1136/emj.2003.008458
Silva, A., & Isbister, G. K. (2020). Current research into snake antivenoms, their mechanisms of action and applications. Biochemical Society Transactions, 48(2), 537-546. https://doi.org/10.1042/BST20190739
Silva, A., Gunawardena, P., Weilgama, D., Maduwage, K., & Gawarammana, I. (2012). Comparative in-vivo toxicity of venoms from South Asian hump-nosed pit vipers (Viperidae: Crotalinae: Hypnale). BMC Research Notes, 5(1), Article 471. https://doi.org/10.1186/1756-0500-5-471
Sofyantoro, F., Yudha, D. S., Lischer, K., Nuringtyas, T. R., Putri, W. A., Kusuma, W. A., ... & Swasono, R. T. (2022). Bibliometric analysis of literature in snake venom-related research worldwide (1933–2022). Animals, 12(16), Article 2058. https://doi.org/10.3390/ani12162058
Suchonwanich, N., & Wananukul, W. (2018). Improving access to antidotes and antivenoms, Thailand. Bulletin of the World Health Organization, 96(12), Article 853. https://doi.org/10.2471/BLT.18.217075
Tan, C. H., Leong, P. K., Fung, S. Y., Sim, S. M., Ponnudurai, G., Ariaratnam, C., ... & Tan, N. H. (2011). Cross neutralization of Hypnale hypnale (hump-nosed pit viper) venom by polyvalent and monovalent Malayan pit viper antivenoms in vitro and in a rodent model. Acta Tropica, 117(2), 119-124. https://doi.org/10.1016/j.actatropica.2010.11.001
Tohamy, A. A., Mohamed, A. F., Moneim, A. E. A., & Diab, M. S. (2014). Biological effects of Naja haje crude venom on the hepatic and renal tissues of mice. Journal of King Saud University-Science, 26(3), 205-212. https://doi.org/10.1016/j.jksus.2014.01.003
Uko, S. O., Malami, I., Ibrahim, K. G., Lawal, N., Bello, M. B., Abubakar, M. B., & Imam, M. U. (2024). Revolutionizing snakebite care with novel antivenoms: Breakthroughs and barriers. Heliyon, 10(3). Article e25531. https://doi.org/10.1016/j.heliyon.2024.e25531
Vaara, S. T., Ostermann, M., Bitker, L., Schneider, A., Poli, E., Hoste, E., ... & Bellomo, R. (2021). Restrictive fluid management versus usual care in acute kidney injury (REVERSE-AKI): A pilot randomized controlled feasibility trial. Intensive Care Medicine, 47(6), 665-673. https://doi.org/10.1007/s00134-021-06401-6
Van Oirschot, J., Ooms, G. I., Okemo, D. J., Waldmann, B., & Reed, T. (2021). An exploratory focus group study on experiences with snakebites: Health-seeking behaviour and challenges in rural communities of Kenya. Transactions of The Royal Society of Tropical Medicine and Hygiene, 115(6), 613-618. https://doi.org/10.1093/trstmh/trab059
Variawa, S., Buitendag, J., Marais, R., Wood, D., & Oosthuizen, G. (2021). Prospective review of cytotoxic snakebite envenomation in a paediatric population. Toxicon, 190, 73-78. https://doi.org/10.1016/j.toxicon.2020.12.009
Villalta, M., Sampaio, T. L., Lima, D. B., Jorge, A. R. C., Alves, R. S., Monteiro, H. S. A., ... & Gutiérrez, J. M. (2019). Nephrotoxicity induced by the venom of Hypnale hypnale from Sri Lanka: Studies on isolated perfused rat kidney and renal tubular cell lines. Toxicon, 165, 40-46. https://doi.org/10.1016/j.toxicon.2019.04.014
Wade, J., Rimbault, C., Ali, H., Ledsgaard, L., Rivera-de-Torre, E., Abou Hachem, M., ... & Laustsen, A. H. (2022). Generation of multivalent nanobody-based proteins with improved neutralization of long α-neurotoxins from elapid snakes. Bioconjugate Chemistry, 33(8), 1494-1504. https://doi.org/10.1021/acs.bioconjchem.2c00220
Waiddyanatha, S., Silva, A., Siribaddana, S., & Isbister, G. K. (2019). Long-term effects of snake envenoming. Toxins, 11(4), Article 193. https://doi.org/10.3390/toxins11040193
Waiddyanatha, S., Silva, A., Weerakoon, K., Siribaddana, S., & Isbister, G. K. (2023). Does snake envenoming cause chronic kidney disease? A cohort study in rural Sri Lanka. Clinical Toxicology, 61(1), 47-55. https://doi.org/10.1080/15563650.2022.2147843
Wijewickrama, E. S., Mohamed, F., Gawarammana, I. B., Endre, Z. H., Buckley, N. A., & Isbister, G. K. (2021). Serum and urinary biomarkers for early detection of acute kidney injury following Hypnale spp. envenoming. PLoS Neglected Tropical Diseases, 15(12), Article e0010011. https://doi.org/10.1371/journal.pntd.0010011
Xie, C., Albulescu, L. O., Bittenbinder, M. A., Somsen, G. W., Vonk, F. J., Casewell, N. R., & Kool, J. (2020). Neutralizing effects of small molecule inhibitors and metal chelators on coagulopathic Viperinae snake venom toxins. Biomedicines, 8(9), Article 297. https://doi.org/10.3390/biomedicines8090297
Zhang, L., Chen, Z., Diao, Y., Yang, Y., & Fu, P. (2015). Associations of fluid overload with mortality and kidney recovery in patients with acute kidney injury: A systematic review and meta-analysis. Journal of Critical Care, 30(4), Article 860.e7-860.e13. https://doi.org/10.1016/j.jcrc.2015.03.025
Zhang, L., Kang, Y., Fu, P., Cao, Y., Shi, Y., Liu, F., ... & Qin, W. (2012). Myoglobin clearance by continuous venous-venous haemofiltration in rhabdomyolysis with acute kidney injury: A case series. Injury, 43(5), 619-623. https://doi.org/10.1016/j.injury.2010.08.031
Zhu, H., Pan, Y., Tai, Z., Wang, M., Liu, X., Yu, X., & He, Q. (2025). Epitope-based antibody development against metalloproteinases and phospholipases A2 from Deinagkistrodon acutus venom. Journal of Venomous Animals and Toxins Including Tropical Diseases, 31, Article e20240060. https://doi.org/10.1590/1678-9199-JVATITD-2024-0060
Downloads
Published
How to Cite
License
Copyright (c) 2025 Journal of Current Science and Technology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.